Dry Eye
Dry eye disease is possibly the most common eye condition that we see in clinical practice. Dry eye occurs when the eyes do not produce enough tears or when the tears evaporate too quickly. Tears are essential for maintaining comfortable clear vision, and a healthy ocular surface. When the tear film becomes unstable, a range of symptoms can develop, including burning, stinging, fluctuating vision, redness, and a gritty “sandy” sensation.
Types of Dry Eye
Dry eye has been broadly divided into two main types, although many patients experience features of both and the newest classification further identifies the clinical drivers of this condition.
Aqueous-deficient dry eye (ADDE):
This occurs when the lacrimal glands fail to produce enough of the watery (aqueous) component of tears. It is commonly associated with autoimmune conditions such as Sjögren’s syndrome and rheumatoid arthritis, but may also result from age-related gland dysfunction.
Evaporative dry eye (EDE):
This form arises when tears evaporate too quickly, usually due to Meibomian gland dysfunction (MGD). These oil-producing glands in the eyelids may become blocked or inflamed, reducing the lipid layer of the tear film that slows evaporation. Environmental factors such as wind, air-conditioning and extended screen time also worsen evaporation.
Risk Factors and Causes
Dry eye can develop from a combination of lifestyle, environmental and medical factors. Common risks include:
Ageing: Tear production naturally decreases with age.
Hormonal changes: Particularly in women during menopause.
Screen time: Reduced blinking during digital device use increases evaporation.
Contact lens wear or prior eye surgeries (e.g. LASIK): Can destabilise the tear film and affect the corneal nerves.
Medications: Antihistamines, antidepressants, beta-blockers, and diuretics may reduce tear production.
Autoimmune disease: Conditions like Sjögren’s syndrome impair lacrimal gland function.
Eyelid problems: Incomplete blinking or lid disease contributes to MGD.
Environmental exposure: Air-conditioning, heating, dusty environments, wind, and smoke.
Tests Used to Diagnose Dry Eye
An experienced optometrist or ophthalmologist will perform a combination of specialised tests to assess tear quality, quantity and ocular surface health:
Ocular surface staining (second image): Dyes such as fluorescein or lissamine green show areas of dryness or damage.
Meibomian gland evaluation (third image): Uses expression or meibography imaging to assess gland structure and oil quality.
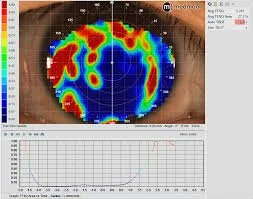
Tear break-up time (TBUT) (bottom image): Measures tear film stability by timing how quickly dry patches appear after blinking.
Schirmer test: Measures tear volume by placing a small paper strip under the lower eyelid.
Osmolarity testing: Detects increased salt concentration in tears, a hallmark of dry eye disease.
Treatment Options
Dry eye management is tailored to the underlying cause and severity. Common treatments include:
Lubricating eye drops: Preservative-free artificial tears replenish moisture. Drops containing oils or lipids can also help prevent evaporation of the tear film.
Warm compresses and lid hygiene: Help treat Meibomian gland dysfunction and improve the lipid layer.
Anti-inflammatory therapy: Steroid drops, cyclosporine or lifitegrast reduce inflammation and improve tear production.
Bandage or scleral contact lenses: Help protect the eye from the desiccating or drying effects of air by acting as a barrier. Scleral lenses also maintain a layer of moisture beneath the lens which helps hydrate the ocular surface.
Punctal plugs: Tiny plugs inserted into tear ducts to slow drainage and increase tear volume.
In-office treatments: Devices such as intense pulsed light (IPL), LipiFlow, iLux or Radio Frequency (RF) therapy help unblock Meibomian glands.
Environmental and lifestyle changes: Increasing blink rate, using humidifiers, adjusting screen habits and staying hydrated.
Nutritional supplements: Omega-3 fatty acids may support healthy tear composition.
Dry eye is highly manageable with proper diagnosis and a personalised treatment plan. Early intervention not only relieves discomfort but also prevents long-term damage to the ocular surface.
Non-invasive tear break up time. The red areas indicate dry spots developing on the cornea
Meibography evaluating the health of the meibomian glands
Lissamine green staining of the eye